Featured Article:Vitamin D Insufficiency Due to Insufficient Exposure to Sunlight and Related Pathology
By
2010, Vol. 2 No. 12 | pg. 1/1
IN THIS ARTICLE
KEYWORDS
AbstractVitamin D has long been considered important for bone health because it aids in the absorption of calcium into the bone tissue. However, emerging research indicates that vitamin D is critical for other body systems to function properly, greatly increasing the scope of vitamin D’s importance. Because vitamin D is produced primarily by exposure to the sun, and because populations who live in northern latitudes have difficulty producing enough vitamin D due to reduced sun exposure, this essay will focus on the specific effects of vitamin D insufficiency experienced in northern regions such as the Pacific Northwest region of the United States.
Vitamin D Insufficiency and Related PathologyIn overcast regions such as the Pacific Northwest region of the United States, there are certain diseases that have an increased prevalence as compared to other areas of the nation. The climate of the Pacific Northwest during the winter months may lead to a higher incidence of these diseases due to vitamin D insufficiency resulting from a lack of sunlight. Additionally, the widespread use of sunscreen coupled with an indoors-oriented lifestyle leaves many people vulnerable to vitamin D insufficiency. Here we will examine the nature of vitamin D, its importance in various body functions and disease prevention, and methods to improve an individual’s vitamin D level. Properties and Uses of Vitamin D in the BodyVitamin D is not technically a vitamin. In its natural form, it is a prohormone that is created by the body; in contrast, vitamins are substances that are extracted from food and used as nutrients in the body. However, the term “vitamin” is commonly used and will be used in this essay for ease of understanding. Vitamin D is often called “the sunshine vitamin”, and for good reason. It is synthesized in the skin of humans and other mammals when exposed to sunlight. There are four forms of vitamin D. The first form, cholecalciferol, is made by the skin when it is exposed to direct sunlight containing UVB rays. Cholecalciferol is also called vitamin D3, and is used in many supplements and in the fortification of food. The second form of vitamin D, calcidiol, is made from cholecalciferol in the liver and stored in the liver for future use. When blood is drawn to test for serum levels of vitamin D in a patient’s body, it is calcidiol that is being tested. The third form of vitamin D, calcitriol, is made from calcidiol in the kidneys. This is the active form of vitamin D, and it regulates calcium and displays properties that prevent cancer. The fourth form of vitamin D is not made in the body. It is called ergocalciferol, and is synthesized by irradiatng ergosterol with UV radiation. Ergosterol is derived from the ergot fungus. Ergocalciferol is often used in the supplementation of food, and once in the body it acts identically to cholecalciferol, and can be converted to calcidiol and calcitriol (Blake, 2007).Traditionally, vitamin D has been viewed by researchers and physicians as functioning mainly to maintain bone density and prevent bone loss. Bone-softening diseases which have been attributed to vitamin D deficiency include rickets in children, and osteomalacia, osteopenia, and osteoporosis in adult patients (Moyad, 2009). While it is true that vitamin D plays a significant role in bone health, emerging research suggests that its presence or absence also contributes to the overall health of other body systems, including the immune system, the autoimmune system, the cardiovascular system, and the integumentary system (Hoffman, et al, 2010). However, according to Bordelon, et al (2009), “because the signs and symptoms of vitamin D deficiency are insidious or nonspecific, it often goes unrecognized and untreated.” Factors Influencing Vitamin D EndogenesisHumans evolved near the equator before migrating to distant corners of the prehistoric landmass. Our methods for synthesizing vitamin D were established at that time, and have not yet evolved to compensate for various factors that limit sun exposure. Populations living at a latitude higher than 37° north of the equator in the Northern Hemisphere are at the greatest risk of developing vitamin D deficiency. In the United States, this translates roughly to a line drawn between San Francisco and Richmond, Virginia (Figure 1); anyone living north of that line has such reduced sun exposure in the autumn and winter months as to make vitamin D synthesis nearly impossible. Seattle is at a latitude of 47° north of the equator, which sets the population up for widespread vitamin D insufficiency. Garland (2003) explained that the storage form of vitamin D has a half life of approximately three weeks, so people in northern latitudes become deficient by December if they are relying solely on the sun for their vitamin D.  Figure 1: United States divided above and below 37th parallel James Dowd, M.D. (2009) explained this concept in another way, saying that the ability to make vitamin D in the skin disappears in the autumn and does not return until the following spring. As the leaves fall from the trees, serum vitamin D levels fall as well. In regions that have a winter shorter than ten weeks, this decrease in serum vitamin D may not have any effect on overall health because the body’s stores will be enough to sustain the people who live there. In regions that have a longer winter, however, individuals’ vitamin D stores will be depleted by January. The only form of vitamin D available to these people in the winter comes from fat stores and dietary supplementation. Industrialization has contributed to widespread vitamin D deficiency. Whereas humans used to spend many hours outside every day working in fields, on farms, and (pre-agricultural revolution) hunting and foraging for food, modern humans in industrialized nations work largely indoors. Time is spent commuting in cars, working all day in factories and office buildings, and leisure time is spent in windowless malls, theaters, or restaurants. When venturing out into the sun, the medical establishment has so forcefully encouraged sunscreen use, vitamin D is often not produced even while standing in direct sunlight if sunscreen is used as recommended. In addition to widespread sunscreen use, clothing choices can predict an individual’s serum vitamin D levels. In populations whose cultural or religious garb covers most of their skin, the amount of vitamin D produced in the tiny areas of exposed skin is not enough to meet minimum serum vitamin D levels. Supplementation and dietary inclusion of vitamin D-containing foods is the most realistic recommendation for members of these populations, as increasing sun exposure would require breaking their own societal laws. Research has been done on hair-coated animals such as dairy cows in order to determine the effect of their hair and other coverings on vitamin D synthesis. The purpose of these studies is to examine the assumption that if the cows produce vitamin D in their hair much like humans produce vitamin D in our skin, clothing the cows would obstruct much of the vitamin D production. Hymøller, et al (2010) designed a study that examined dairy cows and varied their level of sun exposure using garments. According to the concluding statements of this study, “the [serum vitamin D level] of the cows after 4 weeks of access to summer sunlight depended heavily on the size of the exposed body surface area. The larger the exposed body surface area of a given cow, […] the higher the serum vitamin D level of the cow at the end of that study.” These findings indicate that cows in their natural state synthesize vitamin D in their hair much like humans synthesize vitamin D in the skin, but adding clothing to the cow interferes with its vitamin D making ability. This experiment serves to underscore the importance of direct sun-to-skin exposure for humans, as clothing prevents or severely limits the amount of vitamin D produced in the skin. Individuals with darker skin tones are naturally more susceptible to vitamin D insufficiency and deficiency. Progressively darker skin is progressively more susceptible to vitamin D insufficiency. Darker skin, which contains more melanin than relatively lighter skin, offers natural protection from UV radiation. This means that darker-skinned individuals need to spend more time in the sun before pre-vitamin D cells in the skin are prompted to produce vitamin D. According to Hall, et. al. (2010), “Melanin, the principal skin pigment, reduces but does not block cholecalciferol [vitamin D3] synthesis. Thus, longer periods of sun exposure are required for equivalent vitamin D synthesis in people of African ancestry compared with those of European ancestry.” Also, “at all latitudes the skin must have enough melanin to block harmful solar UV while letting in enough UVB for vitamin D synthesis. Since the tropical zone has intense year-round sunlight, even very dark skin can produce sufficient vitamin D for the body’s needs. […] however, when dark-skinned humans move to the temperate zone […] their skin now screens out too much UVB and produces too little vitamin D.” (Frost, 2009). According to Cannell (2008), people with dark skin need to spend 5-10 times longer in direct sun exposure than do people with light skin to achieve similar vitamin D production. Additional Factors Influencing Blood Serum Vitamin D LevelsIn addition to individuals who do not produce enough vitamin D in their skin, there are other individuals who may have adequate stores of vitamin D in the body that are not released into the bloodstream. Because vitamin D is a fat soluble vitamin, it is stored in the body’s adipose tissue. In individuals with increased levels of fat, even those who produce or take in the recommended level of vitamin D, more vitamin D is stored on a standby basis, which lowers the amount of vitamin D found in the bloodstream (referred to as “serum level”). According to Hoffman, et al (2010), “studies confirm an association between obesity and vitamin D deficiency”. In addition to people who are obese, “other people with chronic conditions may also be at risk of deficiency, and need to consider taking a supplement; these include people […] with fat malabsorption conditions (Crohn’s disease, celiac disease, and cystic fibrosis) and those taking certain medication (anticonvulsants, Colestyramine, colestipol).” (Phillips, 2009). Diseases Influenced by Vitamin D InsufficiencyThe medical establishment has traditionally viewed vitamin D as being necessary for bone health and not much else. While there has been a recent growth in research regarding vitamin D’s involvement in other body systems, it remains one of the most important nutrients for skeletal health. When the United States began supplementing milk products with vitamin D in the 1920s, the reason to do so was to prevent rickets in children (Mittelstaedt, 2008). Rickets is a condition found in developing and growing bones in which there is not enough calcium for complete ossification. Research at that time found the connection between adequate vitamin D levels and calcium absorption; supplementing the nation’s milk supply has all but eliminated rickets. Children are not the only ones who experience bone softening. Osteomalacia is the same disease as rickets, but it occurs in adults rather than in children. Literally translated, osteomalacia means “the softening of bones”. Bones are living organs, and as such break down and build up bone cells on a constant basis. Osteomalacia occurs with insufficient calcium absorption into the bones as their cells regenerate, and insufficient calcium absorption is caused by insufficient vitamin D levels. Osteoporosis is a more severe bone condition that is heavily influenced by calcium and vitamin D levels. Typically, osteoporosis is a condition of elderly adults, women moreso than men. If a person does not have adequate calcium absorption for a long enough period of time, he or she can develop osteoporosis, which is a condition marked by extremely porous bone tissue. This condition can lead to fractures while performing everyday activities such as sitting, walking up stairs, or carrying groceries. In order to prevent or reverse osteoporosis, an individual would need to get enough vitamin D along with their calcium intake so the calcium can be used in the bones. Osteoporosis is a widespread problem, but is markedly elevated in elderly housebound people, as they receive drastically reduced amounts of sun exposure. For decades, it has been noted that colon cancer rates increase as geographical latitude increases (Figure 2). Initially, this correlation was noted in 1974 by brothers Frank and Cedric Garland in the United States (Mittelstaedt, 2008), and was attributed to Western diet and habits, but subsequent studies controlled for lifestyle factors indicated sunlight levels were at the root of the difference in cancer rates between latitudes (Hoffman, et. al., 2010). Because of the Garland brothers’ research, other studies have been performed that suggest more than a dozen other cancers, including breast and prostate cancer, “appear sensitive to insufficiencies of [vitamin D]” (Mittelstaedt, 2008). According to Garland (2003), avoiding the sun entirely “would not be the best strategy for reducing overall incidence of cancer. Recommending moderate exposure to the sun would be more prudent.” 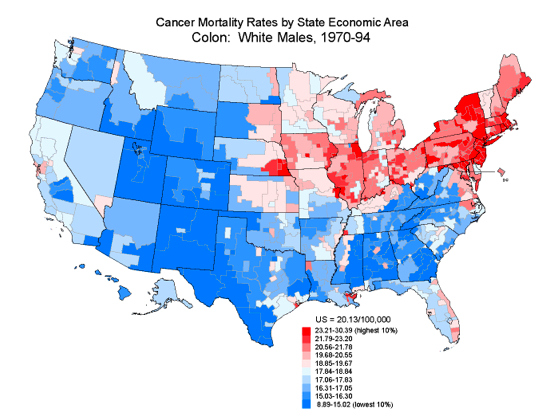 Figure 2: United States Colon Cancer Rates 1970-1994 Asthma is another condition with which vitamin D levels are associated. According to Sutherland, et al (2010), “in asthma, reduced vitamin D levels are associated with impaired lung function, increased airway hyperresponsiveness, and reduced glucocorticoic [inhaled asthma medication] response, suggesting that supplementation of vitamin D levels in patients with asthma may improve asthma severity and treatment response.” Within that same study, Suterland, et al suggest adult patients with asthma whose symptoms do not respond very well to inhaled corticosteroids may benefit from having their serum vitamin D levels tested and supplemented if found to be insufficient. Multiple Sclerosis, which causes progressive nerve damage, has been linked to vitamin D levels. Washington State has one of the highest MS rates in the nation, and it has been theorized that the low levels of solar radiation in the winter contribute to this statistic. However, the body of research regarding MS and vitamin D insufficiency is widely debated, so an understanding that the research is ongoing is important when considering vitamin D’s potential influence on Multiple Sclerosis. Vitamin D also plays a part in diabetes. It has been suggested that “vitamin D supplementation could decelerate the epidemic of type 2 diabetes” (Bell, 2008). We know that obesity is associated with low vitamin D levels, and we also know that low vitamin D levels can be associated with insulin resistance (Hoffman, et al., 2010). According to Liu, et al (2005), in a study of adolescents without diabetes in the United States, “low concentrations of vitamin D were strongly associated with overweight status and abdominal obesity. And after multiple adjustments, vitamin D concentrations were inversely associated with the metabolic syndrome [associated with insulin resistance].” That is to say, low vitamin D levels are correlated with a higher predisposition to insulin resistance, and compensating for those low levels with supplements or sunshine can be correlated with a lower predisposition to insulin resistance and diabetes. The effects of vitamin D insufficiency or deficiency are not purely physical. Studies suggest that depression and other mental illnesses such as schizophrenia and severe bipolar disorder may be influenced by serum levels of vitamin D. According to Cannell (2008), “epidemiological evidence suggests that mental illness has increased as humans have migrated out of the sun and into buildings, cars, and sunblock”. A study performed in 2002 compiled statistics on so-called “insanity” over the past 250 years. Although severe limitations exist in such a study, in that individuals cannot be tested for specific vitamin D deficiencies, a convincing argument was made based on the findings that the current rate of insanity “is not part of the human condition and has increased more than 20 fold in the last 250 years” (Cannell, 2008). Seasonal Affective Disorder, also referred to as SAD, appears to be influenced by a seasonal lack of vitamin D and is prevalent in regions above 40° latitude. In a study conducted by Gloth, et al (1999), 100,000 International Units (IU) of vitamin D improved depression better than light therapy in a small group of patients with SAD. That is to say, improvement of serum vitamin D levels associates strongly with improvement in depression scale scores. Reversing or Preventing Vitamin D Insufficiency to Improve or Preclude PathologySun exposure is the easiest and least expensive way for an individual to increase his or her serum vitamin D level. Not all sun exposure is created equal, however. A widely accepted rule of thumb states that “if your shadow is longer than you are, the sunlight is not intense enough [to trigger vitamin D synthesis in the skin]” (Mittelstaedt). According to Blake (2007), “fifteen minutes of summer sun in a bathing suit makes an average of 20,000 IU of vitamin D—100 times the adequate daily intake. Since vitamin D is stored for long periods, this may be enough vitamin D to last for 100 days.” Depending on where an individual lives and how long their local winter is, this may be enough to carry an individual through the sunless winter months. Limiting the use of sunscreen is another way to increase an individual’s vitamin D level. Within the past thirty years, sunscreen use has been encouraged in order to reduce the incidence of skin cancers. While solar radiation still poses this risk, overcompensation with sunscreen has been shown to severely limit an individual’s capacity to produce naturally-occurring vitamin D. According to Mittelstaedt, “while there is a risk of skin cancer from overexposure to ultraviolet light, […] the benefits of modest sun exposure in preventing serious, hard-to-treat cancers outweighs that risk. Furthermore, […] skin cancer is relatively easy to treat.” A suggested compromise for sunscreen users is to spend five or ten minutes in the midday sun without the sunscreen, then apply as normally directed. This brief amount of exposure is enough to synthesize of weeks’ worth of vitamin D. It is possible to obtain vitamin D through naturally-occurring dietary sources. However, there are very few foods that contain vitamin D, some of which are: cod liver oil (1300 IU per tablespoon); wild salmon (1000 IU per serving); farmed salmon (250 IU); sardines (600 IU); fortified milk or orange juice (100 IU); egg yolk (25 IU); fresh shiitake mushrooms and some organ meats (traces in both) (Mittelstaedt, 2008). Considering that there is a debate regarding the appropriate amount of daily vitamin D, it may or may not be reasonable to obtain all of the necessary vitamin D from dietary sources. The US dietary recommendation for vitamin D is not clearly defined. According to the U.S. Department of Health and Human Services, individuals who are at higher risk of vitamin D insufficiency, such as individuals with dark skin or those who are housebound, should increase their daily intake to 1000 IU, but there is no specified guideline for the daily vitamin D intake for individuals of lower risk. The health.gov website also specifies that “optimal serum 25-hydroxyvitamin D may be as high as 80 nmol/L”, which provides clinicians with a benchmark to measure their patients’ relative risk. Canada has recently increased their RDA to 1000 IU daily year-round for non-white adults, and 1000 IU daily in the fall and winter for white adults. Supplementation is a valid way for many individuals to reach their recommended daily intake of vitamin D. According to Bordelon, et al (2009), “evidence shows that vitamin D supplementation of at least 700 to 800 IU per day reduces fracture and fall rates in adults.” Toxicity of Vitamin DIt is important to note that it is possible to have too much vitamin D in the body. However, the point at which vitamin D becomes toxic is a point of contention. It is widely accepted that vitamin D produced in the skin as a result of sun exposure “is not known to result in toxic levels” (Blake, 2007). This is because levels produced in the skin are self-adjusting based on the body’s needs. Vitamin D toxicity is known as hypervitaminosis D. Extremely high blood levels of vitamin D can cause abnormally high blood calcium levels. This can cause some of the conditions that vitamin D is usually prescribed to prevent, including bone loss. According to Blake (2007), “ long-term overconsumption of vitamin D can cause calcification of organs such as the heart, blood vessels, and the kidneys.” However, vitamin D toxicity is unlikely in healthy adults who are consuming fewer than 10,000 IU of vitamin D through supplements each day. The widely accepted Upper Intake Level (UL) of vitamin D is approximately 2000 IU per day via supplementation, but this figure is being examined as vitamin D’s benefits are being studied more and more. According to Cannell (2008), “One could compare vitamin D toxicity to water intoxication. For example, 8 glasses of water a day is recommended consumption. However, regular consumption of 80 glasses a day can be fatal. So you could say that water has a therapeutic index of 10 (80/8). Most vitamin D experts now say that humans should get about 4,000 units of vitamin D a day (from all sources), but 40,000 units a day will hurt them (over several years). Therefore, vitamin D has a therapeutic index of 10 (40,000/4,000), the same as water. Although we are not saying it is as safe as water, we are saying vitamin D is safe when used in the doses nature uses it.” ConclusionAll of the recent research on vitamin D can be overwhelming, and it is important to remember that vitamin D’s effectiveness in preventing or reversing disease is still being studied. Many of the so-called “latitude studies” are observational studies that “use ambient solar UV radiation as a proxy for latitude and Vitamin D status. For these studies, researchers compare rates of certain major cancers […] to rates of sunlight exposure. This group of research has the liability of being wildly inconsistent.” (Marshall Protocol Knowledge Base, 2010). That is to say, studies that extrapolate data based on correlation may not draw the correct conclusion. A researcher cannot draw conclusions regarding causation simply by looking at a map. It is clear that more research needs to be done in order to establish reliable guidelines on Vitamin D3 levels for all populations. Because Vitamin D3 supplements are very inexpensive, there is likely no pharmaceutical company that will spearhead the research required, and it seems that the Federal Government will eventually need to take up this cause. However, even without further research, it is known that low vitamin D levels can be detrimental, and persons with one or more risk factors would benefit from speaking to their physician about this issue.
Bell, D. (2008, August). The role of vitamin D for obese patients in reversing the type 2 diabetes pandemic. Endocrine Today, 6(15), 4. Retrieved May 27, 2010, from ProQuest Health and Medical Complete. (Document ID: 1534872801). Blake, S. (2007). Vitamins and Minerals Demystified. Blacklick, OH, USA: McGraw-Hill Professional Publishing. p 99. Retrieved May 27, 2010, from http://site.ebrary.com/lib/pima1/Doc?id=10210113&ppg=119 Bordelon, P., Ghetu, M., & Langan, R. (2009). Recognition and Management of Vitamin D Deficiency. American Family Physician, 80(8), 841-6. Retrieved June 13, 2010, from ProQuest Medical Library. (Document ID: 1903280861). Cannell, J.J. (2008). Vitamin D and Mental Illness. Retrieved June 15, 2010 from http://www.vitamindcouncil.org/mentalIllness.shtml. Dowd, J. (11-11-2009). Falling Leaves Means Falling Vitamin D. Retrieved on May 31, 2010 from http://www.thevitamindcure.com/blog/?p=99. Frost, P. (2009). Black-White Differences in Cancer Risk and the Vitamin D Hypothesis. Journal of the National Medical Association, 101(12), 1310-2. Retrieved June 2, 2010, from ProQuest Medical Library. (Document ID: 1923084561). Garland, C. F. (2003). Sun avoidance will increase incidence of cancers overall. British Medical Journal, 327 (7425), 1228. Retrieved June 2, 2010, from ProQuest Medical Library. (Document ID: 479857221). Gloth, F.M. III, Alam, W., Hollis, B.. (1999). Vitamin D versus broad spectrum phototherapy in the treatment of seasonal affective disorder. Journal of Nutritional Health and Aging. 3(1),5-7. Hall, L., Kimlin, M., Aronov, P., Hammock, B., Slusser, J., Woodhouse, L., & Stephensen, C. (2010). Vitamin D Intake Needed to Maintain Target Serum 25-Hydroxyvitamin D Concentrations in Participants with Low Sun Exposure and Dark Skin Pigmentation Is Substantially Higher Than Current Recommendations1,2. The Journal of Nutrition, 140(3), 542-50. Retrieved June 2, 2010, from ProQuest Medical Library. (Document ID: 1992506731). Hoffman, R. (2010, March). What lies behind the vitamin D revolution? The Clinical Advisor: For Nurse Practitioners, 13(3), 31-37. Retrieved May 27, 2010, from ProQuest Nursing & Allied Health Source. (Document ID: 2009224851). Hymøller, L., & Jensen, S. (2010). Vitamin D3 Synthesis in the Entire Skin Surface of Dairy Cows Despite Hair Coverage. Journal of Dairy Science, 93(5), 2025-2029. Retrieved June 13, 2010, from ProQuest Medical Library. (Document ID: 2021690391). Liu, S., Song, Y., Ford, E.S., Manson, J.E., Buring, J.E., & Ridker, P.M. (December 2005). Dietary Calcium, Vitamin D, and the Prevalence of Metabolic Syndrome in Middle-Aged and Older U.S. Women. Diabetes Care. Retrieved on May 31, 2010 from http://care.diabetesjournals.org/content/28/12/2926.full.pdf+html. Marshall Protocol Knowledge Base. (2010). Latitude Studies on Vitamin D and Disease. Retrieved June 21, 2010 from http://mpkb.org/home/pathogenesis/vitamind/latitude. Mittelstaedt, M. (March 8, 2008). The Vitamin D Miracle: Is It For Real? Retrieved May 31, 2010 from http://www.sott.net/articles/show/150704-The-vitamin-D-miracle-Is-it-for-real. Moyad, M. (2009). Vitamin D: A Rapid Review. Dermatology Nursing, 21(1), 25-30, 55. Retrieved June 13, 2010, from ProQuest Medical Library. (Document ID: 1692586111). Phillips, F. (2009). The functions of vitamin D. Practice Nurse, 38(10), 26-29. Retrieved June 17, 2010, from ProQuest Nursing & Allied Health Source. (Document ID: 1939513211). Sutherland, E., Goleva, E., Jackson, L., Stevens, A., & Leung, D.(2010). Vitamin D Levels, Lung Function, and Steroid Response in Adult Asthma. American Journal of Respiratory and Critical Care Medicine, 181 (7), 699-704. Retrieved May 26, 2010, from ProQuest Medical Library. (Document ID: 2013060011). U.S. Department of Health and Human Services. (2005). Dietary Guidelines for Americans. 19, 20. Retrieved May 31, 2010 from http://www.health.gov/dietaryguidelines/dga2005/document/pdf/DGA2005.pdf. Suggested Reading from Inquiries Journal
Inquiries Journal provides undergraduate and graduate students around the world a platform for the wide dissemination of academic work over a range of core disciplines. Representing the work of students from hundreds of institutions around the globe, Inquiries Journal's large database of academic articles is completely free. Learn more | Blog | Submit Latest in Health Science |